
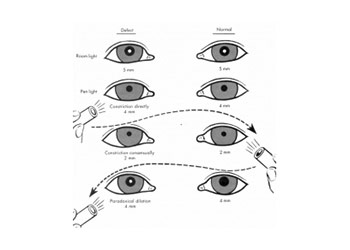
If you’ve been to one since you’ve reached your adult size, your doctor should have an accurate measurement on file give them a call and ask if they can provide your IPD measurement in millimeters. The most accurate IPD measurement you’ll be able to get is from an eye-doctor. If you don’t have access to one of the above devices for an automatic measurement, here’s other ways you can measure your IPD. The GCS is designed to assess the integrity of.Other Ways to Measure Your IPD Image courtesy Will Folsom ( CC BY 2.0) The GCS was originally developed to monitor the progress of patients with an acute head injury however, it is now generally considered to be a useful tool for assessing all patients who are potentially at risk of neurological deterioration, regardless of their primary pathology. The layout and appearance of the neurological observation chart incorporating the GCS will vary, depending on the trust in which you work. Recently published guidelines for the management of patients with head injuries (National Institute for Clinical Excellence (NICE) 2003) stipulate the use of the GCS for assessment and classification of all head-injured patients.Īlthough there have been some useful articles on the GCS tool (Ellis and Cavanagh 1992, Shah 1999, Woodward 1997a, b, c, d), benchmarking standards have relied on consensus and the expertise of skilled nurses from neuroscience units throughout the UK. * Limb movements (motor and sensory function). The neurological observation chart incorporating the GCS is well established both nationally and internationally (Teasdale and Jennett 1974) as the primary tool used by nurses to make quick, repeated evaluations of several key indicators of neurological status (Auken and Crawford 1998): Accurate assessment and prompt action when needed can improve the eventual outcome, not just in terms of survival but also by minimising the degree of residual neurological deficit. Nurses working in these areas need to be able to perform a basic neurological assessment accurately and understand the significance of the findings. Many patients are admitted to neurosurgical units from general clinical areas such as medical units or accident and emergency departments. * Perform a neurological assessment, using the GCS, pupil reaction, limb responses and vital signs, and interpret the findings. * Assess a patient's level of consciousness by evaluating three behavioural responses: eye opening, verbal response and motor response. * Outline the rationale for using the GCS. After reading this article you should be able to:
#Pupil size chart to scale how to#
It explains how to complete the neurological observation chart, which includes the GCS, accurately, safely and consistently. It should be of value to all nurses who care for patients at risk of neurological deterioration. This article aims to raise awareness of basic neurological observations, namely the Glasgow Coma Scale (GCS), pupil reaction, limb responses and vital signs.

#Pupil size chart to scale archive#
For related articles and author guidelines visit the online archive at and search using the keywords. This article has been subject to double-blind review. These keywords are based on the subject headings from the British Nursing Index. Glasgow Coma Scale Neurological assessment Observations Vital signs This article explains the correct use of the chart and how to interpret the findings. The primary tool used by nurses to assess a patient's neurological status is the neurological observation chart incorporating the Glasgow Coma Scale. NS289 Waterhouse C (2005) The Glasgow Coma Scale and other neurological observations.


 0 kommentar(er)
0 kommentar(er)
